ABCs of Quality Improvement
Pediatricians have a unique opportunity to prevent and identify physical and mentaldisorders in children and adolescents.
Delivery of best care makes a number of demands on practices, including:
translating best evidence guidelines into daily practice,
adapting to an increase in chronic conditions and behavioral and mental health disorders of childhood,
responding to increasing expectations to measure, report on, and continually improve quality of care,
meeting payor expectations to meaningfully incorporate electronic records and to transform practices into patient centered medical homes.1
1 Adapted from The National Improvement Partnership Network: State-Based Partnerships That Improve Primary Care Quality Shaw, Judith S. et al., Academic Pediatrics, Volume 13, Issue 6, S84 - S9
Enter the Alabama Child Health Improvement Alliance
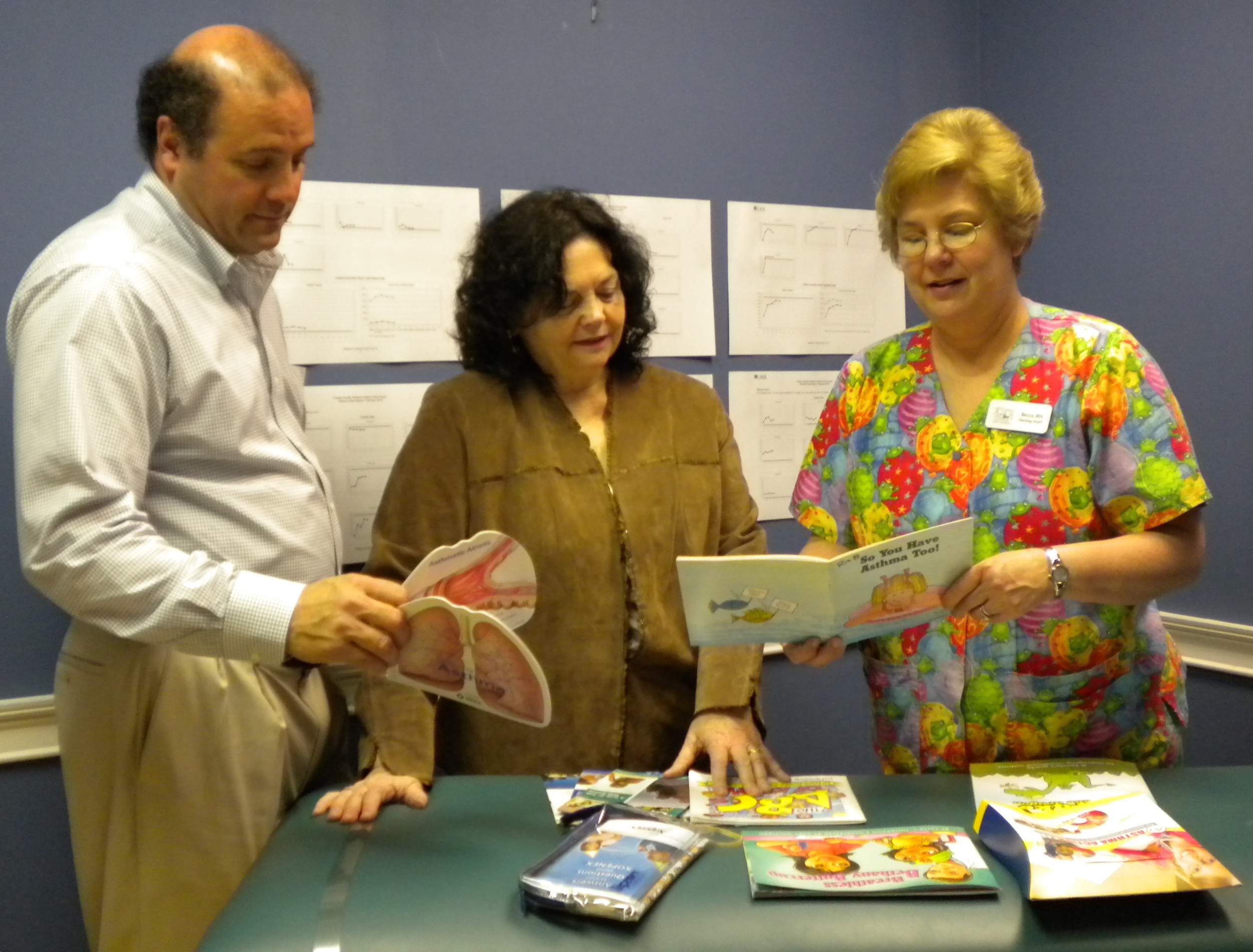
The Alabama Child Health Improvement Alliance (ACHIA), founded by the Alabama Chapter-AAP in 2013, supports pediatric and family medicine practices in improving the care delivered to infants, children and adolescents.
ACHIA develops and implements practice collaboratives around areas of care in need of improvement such as improving obesity prevention and treatment or increasing screening to identify children at risk of developmental delay at ages where intervention is most beneficial. These collaboratives are approved for Maintenance of Certification Part 4 by the American Board of Pediatrics.
ACHIA supports practice-based improvement with faculty experts in targeted content areas, quality improvement coaching to implement workflow changes, technical assistance in collecting and interpreting quality improvement data, as well as information about coding the level of care delivered.
Shift Happens: What is Continuous Quality Improvement?
Continuous Quality improvement (CQI) consists of systematic and continuous actions that lead to measurable improvement in health care services and the health status of targeted patient groups.
CQI encourage healthcare team members to continuously ask the questions, “How are we doing?” and “Can we do it better?” (Edwards, 2008). The Institute of Medicine's (IOM) Exit Disclaimer, which is a recognized leader and advisor on improving the nation's health care, defines quality in health care as a direct correlation between the level of improved health services and the desired health outcomes of individuals and populations.
A good introduction to quality improvement is the Model for Improvement brief videos (Clips 1 and 2, below) that provide a simple look at how providers approach QI in practice - which is the foundation for ACHIA's collaboratives.
The Institute of Medicine’s (IOM) 1999 report To Err is Human: Building a Safer Health Care System identified gaps in quality in US healthcare by reporting that found 48,000-98,000 Americans die each year due to preventable medical errors. The IOMs 2001 subsequent report, Crossing the Quality Chasm: Health Care in the 21st Century provided a framework to improve medical care by following six guiding principles: that care be safe, effective, patient centered, timely, efficient and equitable.